This story is about the microbial theory of Alzheimer’s disease. Why am I writing about it? I am writing about it because it’s like unraveling a detective plot. There is a disease that they say a lot of people have — and that is caused, they say, by amyloid deposits in the brain. But then it turns out that the currently widely accepted narrative about this disease is based on forged research.
Then more research shows up suggesting that amyloid deposits might be a reaction, an immune response to something, even though nobody seems to know exactly to what.
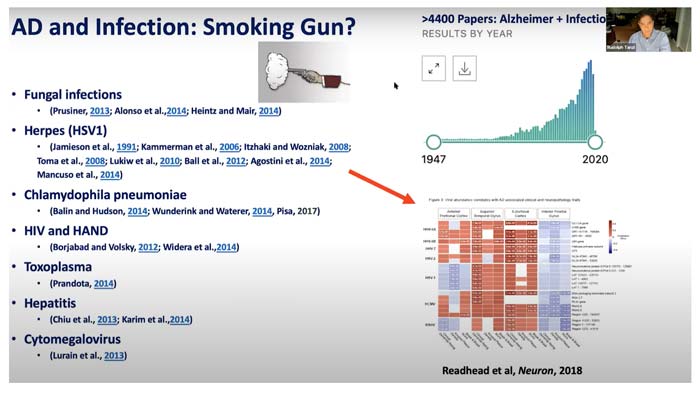
Then there are general debates about brain microbiome, an admission that our brain is not sterile, and also growing evidence that a number of microorganisms (including bacteria, fungi, and especially parasites that are more common that we westerners give ourselves credit for) can cause a significant inflammatory response in the brain — resulting in symptoms associated with Alzheimer’s disease.
To add to the complexity of the plot, it is probably logical to assume that the microbes — whichever microbes they are — would have a much harder time causing wreckage if our bodies and our environments weren’t poisoned so devastatingly, so through and through. But environmental toxicity is a part of our lives, it is superimposed on us (and COVID “vaccines” didn’t help).
And because we are living in a world that unavoidably poisons us as we go about daily lives (hi, glyphosate, synthetic biology, geoengineering, aluminum, shedding, and EMFs!), I am writing this because it is practical to try and understand how those microbial interactions work in our current conditions and maybe acknowledge the fact that we don’t live in an ideal world where it’s easy to maintain the microbiome and the immunity of supergods.
We are like trees in a poisoned desert, stretching our branches toward the sun no matter what, fighting for life no matter what, and we will be stronger if we look at all factors involved.
(Yes yes, I am nodding at the famous debate about germ vs. terrain that — in its extreme form — seeks to strike down the concept of contagion as such, which to my senses is rather contrived since both germs and terrain exist — in fact they are rather intermixed — and they both play a role in this very complex world of ours.)
On a side note, to illustrate my general point that our understanding of the world tends to evolve and that it’s good to keep an open mind, the scientific community just recently discovered a whole new part of the brain!
Anyway, the biology and the etiology of AD is one part of the detective plot. But in parallel to the plot about the inner workings of our bodies, there is another detective story brewing underneath. That other plot is about financial and political factors that determine the timing of narrative “release.”
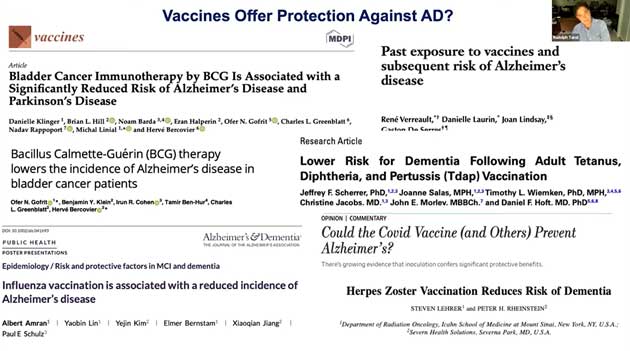
And today, as the story of the infection possibly causing AD is quietly brewing in the mainstream (National Institute of Aging, Harvard, JAMA, Guardian, BBC, NPR, CBS, the New York Times), there is talk about using vaccines to prevent pathogen-driven AD. There is even talk about flu vaccines preventing AD! Case in point:
“Two studies presented Monday (July 27) at this year’s virtual Alzheimer’s Association International Conference have demonstrated that flu and pneumococcal vaccines are linked with a lower risk of Alzheimer’s disease.
In both studies, individuals who had received at least one vaccination — a flu shot in one study, and a pneumonia vaccine with or without a flu shot in the second — were less likely to be diagnosed with Alzheimer’s later in life. While the studies are slightly different, their similar conclusions suggest that vaccines may play a broader role in strengthening a person’s lifelong resistance to some diseases.”
Also this.
In meanwhile though, the increasing popularity of the “infectious” AD hypothesis didn’t hold the FDA back from granting a fast-track designation to UB-311, an anti-Aβ antibodies-based “vaccine for Alzheimer’s disease made by biotechnology company Vaxxinity,” which they did in May 2022. Better safe than poor! As of January 2023, the company is seeking a partner for Phase 3 development, and has not registered nor begun a large trial of UB-31.
On the infectious side, there is talk about shingles being to blame for AD — and we know about the new push for the shingles vaccine. If the narrative about that link gets favored, we can only imagine the pressures mounted to get everyone vaccinated against shingles in order to prevent AD and becoming a burden on your loved ones and the state, etc. (Or else MAID?)
In a separate subplot, there is also ongoing research into vaccines against Toxoplasma gondii, the intracellular parasite that could be complicit in AD. The vaccines they’ve been working on may come in different forms, including a DNA vaccine and — for animals, currently — as a rather sour-sounding oral vaccine consisting of a genetically modified version of the parasite. (Unrelatedly, here’s one for Lyme that could “come as soon as 2025.” They are on a roll!)
One could say, so what, there is always talk about vaccines against everything under the sun, they can talk! Yes, that’s true, there is always talk about them since the “v-word” is a famous cash cow and a required talking point in the mainstream.
However, in the light of the past three years and in the context of an objectively existing malaise (dementia, in this case) and an objectively prevalent but often misdiagnosed and misunderstood parasite (Toxoplasma g.), that direction of conversation alarms me quite a bit.
And methinks that it’s better for us to educate ourselves and start thinking it through now. It would also tremendously help if the doctors with honest minds decided to investigate it thoroughly with our actual health in mind, before the robo-eyed ones try to force a new “health countermeasure” on us that doesn’t help and that we hadn’t asked for.
And that is why I think we should talk about it now. On my end, I would like to loudly proclaim a divorce of exploring how things work from anyone’s push for “vaccines” — and it is easier to do that preemptively, before the syringe is prepared, and the conversation about infectious AD goes full mainstream.
What Is Alzheimer’s Disease, Anyway?
Given the prevalence of Alzheimer’s disease in elders and the amount of funding the topic receives, one would think that at the very least, we’d have a reliable definition of the disease and a solid way to diagnose. But not so fast, soldier, not so fast.
Let’s start with the basics. Per Science, “one of its biggest mysteries is also its most distinctive feature: the plaques and other protein deposits that German pathologist Alois Alzheimer first saw in 1906 in the brain of a deceased dementia patient.
In 1984, Aβ [protein amyloid beta] was identified as the main component of the plaques. And in 1991, researchers traced family-linked Alzheimer’s to mutations in the gene for a precursor protein from which amyloid derives. To many scientists, it seemed clear that Aβ buildup sets off a cascade of damage and dysfunction in neurons, causing dementia. Stopping amyloid deposits became the most plausible therapeutic strategy.”
And according to the NIH, “higher levels of beta-amyloid are consistent with the presence of amyloid plaques, a hallmark of Alzheimer’s disease.” Additionally, “most widely used CSF [cerebrospinal fluid] biomarkers for Alzheimer’s disease measure beta-amyloid 42 (the major component of amyloid plaques in the brain), tau, and phospho-tau (major components of tau tangles in the brain, which are another hallmark of Alzheimer’s).”
The societal handling of Alzheimer’s is a microcosm reflecting the macrocosm of our culture and economics at large. And so, If I were to think this through like an intellectually honest five-year-old child, I would ask these questions:
• When Alois Alzheimer, the German pathologist who gave the disease its name, discovered those plaques in the deceased patient’s brain, could he or anyone else know that the plaques he had found were the cause of dementia and not a byproduct of something else that was going on, like an inflammatory presence of bacteria or parasites?
• An extracurricular question? Why do the scientists of today like to assume that our bodies are broken machines — and not wise wonders who usually do things for a reason? Why?
• Later, when the scientists claimed that they had found a reliable biomarker of Alzheimer’s disease, did they gain a new insight into the causation of AD — or did they just make a conventional industry-wide agreement to use the AD diagnosis whenever the biomarker was found?
(Incidentally, I know the answer to that question. It’s the latter. I learned about it in 2019 at a legal conference about the ethics of AI (or something along those lines) and I remember how perplexed I was to learn from a doctor panelist that once the AD biomarker had been adopted as the primary way to diagnose the disease, some patients with the biomarker but without dementia would be diagnosed as AD, while other patients with dementia but without the biomarker would be left with a “mystery disease.”) Little did I know how “interesting” the following year of 2020 would be in that sense!
• And what if Alzheimer’s disease is not really one disease but an umbrella term for a heap of conditions caused perhaps by inflammation in the brain, and what if — so shocking and novel, I know! — inflammation can be caused by multiple factors, and when the scientists make confident statements about the cause of Alzheimer’s Disease, they are mostly poking their fingers into the sky and puffing cheeks to justify their grants — while having very little idea about what causes what?
Speaking of Puffing Cheeks, the Fraud
“Over the last two decades, Alzheimer’s drugs have been notable mostly for having a 99% failure rate in human trials.
It’s not unusual for drugs that are effective in vitro and in animal models to turn out to be less than successful when used in humans, but Alzheimer’s has a record that makes the batting average in other areas look like Hall of Fame material … And now we have a good idea of why.
Because it looks like the original paper that established the amyloid plaque model as the foundation of Alzheimer’s research over the last 16 years might not just be wrong, but a deliberate fraud.”
As a result, in late 2022, an “ultimate” trial of the amyloid hypothesis was launched.
Infectious Hypothesis: A One-Million-Dollar Challenge
In early 2018, Dr. Leslie Norins of Alzheimer’s Germ Quest (their website is no longer live) announced a one-million-dollar challenge award for the scientist who would find the germ causing Alzheimer disease.
The challenge lasted three years, and in February 2021, the press release said that “eight final honorees will divide $200,000 for meritorious entries in Alzheimer’s Germ Quest’s ‘$1 Million Challenge.’
However, nobody provided persuasive-enough evidence that a particular infectious agent was the sole cause of Alzheimer’s disease, so the grand prize of $1 million will not be awarded … Six microorganisms were nominated: herpes, toxoplasma, Borrelia, mycobacteria, H. pylori, and P. gingivalis.”
Toxoplasma Gondii
I wrote about this tricky parasite last year, and I think it calls for a good look in the context of its prevalence in the population and the glaring gap between the recent toxoplasma research and the outdated information that they seem to teach doctors in medical school.
In the AD research world, toxoplasma is getting less of a spotlight than it deserves — but in the toxoplasma research world, its connection to Alzheimer’s has come up multiple times. Here is the summary of what my earlier article said:
• At least one third of all people on Earth are infected with the parasite Toxoplasma gondii, averaging from 11-20% in the United States to 50% and higher in some Western European countries
• The parasite has been implicated in ocular issues, schizophrenia, epilepsy, Alzheimer’s disease and various other neurological disorders, as well as in heart disease, pneumonia, recurrent headaches, even cancer; it is also known for causing psychological changes in its hosts
• While the official word is that most toxoplasma infections are harmless and asymptomatic, the impact of the parasite could be much more devastating than the current mainstream medical convention presumes; it may also be cross-reacting with the spike protein and possibly contributing to the mystery of “long COVID”
• According to recent research and clinical evidence, toxoplasma tissue cysts, previously considered harmless in immunocompetent patients, are capable of causing major health issues without converting to the cell-blasting form
• Commonly used antibody tests can only detect antibodies for the “tachyzoite” (cell-blasting) form of the parasite but not the “bradyzoite” (tissue cyst) form
The State of the Alzheimer’s ‘Infectious’ Hypothesis
According to a 2020 paper tilted, “Infectious hypothesis of Alzheimer disease”:
“The infectious hypothesis proposes that a pathogen (virus, bacteria, prion, etc.) is the root cause of AD [2]. The hypothesis is supported by evidence that some pathogens, such as herpesviruses and certain bacterial species, are found more commonly in AD patients. There is some variation within the infectious hypothesis field as to how an infectious pathogen explains the pathological hallmarks of AD.
Direct infection and eventual death of central nervous system (CNS) cells by pathogens could explain the cognitive deficits and heightened inflammation found in AD [3].
The relationship between inflammation and the AD hallmarks has long been recognized, with inflammation hypothesized to cause tissue damage, leading to protein aggregates such as Aβ plaques and tangles, which in turn can lead to more inflammation [4].”
“This cascade could be initiated by a number of endogenous and external factors, including microbial pathogens. Alternatively, Aβ and tau may be the products of normal responses to infection, intended to sequester threats to the CNS [5].
Accumulation of Aβ and tau could then occur when the generation of the aggregates outpaces clearance by the microglia in the brain, a process brought about by the natural process of aging [5] …
The aggregates themselves have shown to trigger neuroinflammation as well [6]. Recent findings have highlighted a number of pathogens as potential drivers of AD, but the family of pathogens most investigated is the herpesviruses [7].”
And here is a 2021 BBC story titled, “Alzheimer’s: The heretical and hopeful role of infection”:
“To date, the most compelling evidence for the infection hypothesis comes from a large study in Taiwan, published in 2018, which looked at the progress of 8,362 people carrying a herpes simplex virus. Crucially, some of the participants were given antiviral drugs to treat the infection.
As the infection hypothesis predicted, this reduced the risk of dementia. Overall, those taking a long course of medication were around 90% less likely to develop dementia over the 10-year study period than the participants who had not received any treatment for their infection.
Scientists studying the infection hypothesis have also started making some headway in explaining the physiological mechanisms. Their explanation centres on the surprising discovery that amyloid beta can act as a kind of microbicide that fights pathogens in the brain.
Studies by Fulop and others, for instance, show that the protein can bind to the surface of the herpes simplex virus. This seems to entrap the pathogen with a web of tiny fibres and prevents it from attaching to cells. In the short term, this could be highly advantageous, preventing the infection from spiralling out of control so that it poses an immediate danger to someone’s life.
But if the pathogen is repeatedly reactivated during times of stress, the amyloid beta could accumulate in the toxic plaques, harming the cells it is meant to be protecting.
As interest in the infection hypothesis has grown, scientists have started to investigate whether any other pathogens may trigger a similar response — with some intriguing conclusions. A 2017 study suggested that the virus behind shingles and chickenpox can moderately increase the risk of Alzheimer’s disease.
There is also evidence that Porphyromonas gingivalis, the bacterium behind gum disease, can trigger the accumulation of amyloid beta, which may explain why poor dental health predicts people’s cognitive decline in old age. Certain fungi may even penetrate the brain and trigger neurodegeneration. If the causal role of these microbes is confirmed, then each finding could inspire new treatments for the disease.”
And the screenprint below is from a 2021 presentation by the National Institute of Aging under NIH.
What About Infectivity?
The funny thing is that billions of dollars in funding later, the honest answer is that nobody knows. That’s the humbling part. The earlier mainstream conviction is that it is obviously not infectious because it’s caused by amyloid plaques. With that hypothesis possibly on its way out, we are back to the drawing board.
When Dr. Leslie Norins announced his one-million-dollar challenge award, he mentioned a few studies that suggested an infectious route.
A 2010 study published in the Journal of Neurosurgery showed that neurosurgeons die from Alzheimer’s at a nearly 2 1/2 times higher rate than the general population. Another 2010 study, published in The Journal of the American Geriatric Society, found that people whose spouses have dementia are at a 1.6 times greater risk for the condition themselves.
And if Toxoplasma gondii has anything to do with it, then up until a certain point, there were papers published showing possible horizontal transmission (here and here) — but then they stopped. Was it because it was concluded that horizontal transmission did not exist? Was it because there was nothing lucrative to sell, while the symptoms could be blamed on something else? I don’t know.
But in any case, the most insane idea in my book would be to not hug our loved ones, Alzheimer’s or not.
About the Author
To find more of Tessa Lena’s work, be sure to check out her bio, Tessa Fights Robots.
