Altering the chemical properties of an anti-nausea drug enables it to enter an interior compartment of the cell and provide long-lasting pain relief, according to a new study led by researchers at NYU College of Dentistry’s Pain Research Center.
The study, published in the Proceedings of the National Academy of Sciences (PNAS), illustrates how pain signaling occurs inside cells rather than at the surface, highlighting the need for drugs that can reach receptors within cells.
G protein-coupled receptors (GPCRs) are a large family of proteins that regulate many processes in the body and are the target of one third of clinically used drugs. A subset of these receptors plays an important role in pain, including the neurokinin-1 (NK1) receptor, which is activated by a pain-transmitting neuropeptide called substance P.
Several FDA-approved drugs that target the NK1 receptor are used to prevent nausea and vomiting associated with chemotherapy or surgery. Scientists previously hoped that the NK1 receptor would be a promising target for treating pain-;but drugs targeting the receptor failed to control pain in clinical trials in the 1990s and early 2000s.
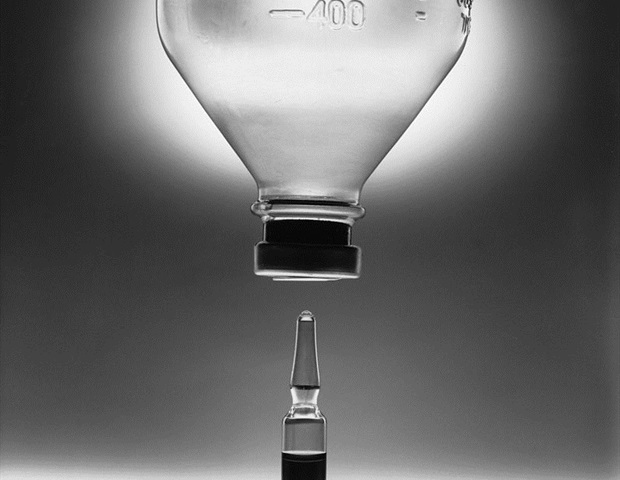
One reason why drugs targeting the NK1 receptor may not have been effective against pain is that most drugs block receptors at the surface of cells. However, researchers at the NYU Pain Research Center have shown that GCPRs signal pain not from the surface of cells, but from compartments inside the cell called endosomes.
Sustained signaling in endosomes is necessary for the hyperexcitability of pain-sensing neurons involved in chronic pain. As a result, treating pain may require the development of drugs that penetrate cells, are retained in endosomes, and disrupt signaling inside the cell.”
Nigel Bunnett, professor and chair of the Department of Molecular Pathobiology at NYU College of Dentistry and the study’s senior author
In the PNAS study, the researchers focused on two drugs, aprepitant and netupitant, both NK1 receptor antagonists used to prevent nausea and vomiting. Studying NK1 receptors in the lab has the benefit of clinically available drugs that target the receptor, but also comes with challenges, as there are large differences between the NK1 receptor in mice and humans. To overcome this, the researchers genetically modified mice to express the human NK1 receptor.
Bunnett and his colleagues had previously shown that encapsulating aprepitant in nanoparticles could deliver the drug to endosomes to block pain, but in this study, aprepitant only briefly disrupted endosomal signaling in cellular studies and stopped pain in mice for short periods.
Modifying the second drug, netupitant, held much more promise. The researchers changed the chemical properties of the drug to make it more capable of penetrating a cell’s lipid membrane. They also altered the charge on the molecule within an acidic environment so that once the drug entered the acidic environment of an endosome, it would stay trapped inside and accumulate.
These changes allowed the modified netupitant to readily penetrate cells to reach the endosome and block signaling of the NK1 receptor in endosomes with a much more prolonged effect in cells. The altered netupitant also had a more potent and long-lasting analgesic effect in mice than aprepitant and the regular form of netupitant.
In another experiment, the researchers studied mice with a different type of NK1 receptor on the outer membrane of the cell, rather than inside. These mice were more resistant to pain than those with human NK1 receptors inside the cell, illustrating the importance of endosomes in signaling pain and the need for treatments that can penetrate cells.
The researchers are continuing this research and other studies in animal models to develop new therapies for pain that block GCPRs in endosomes.
“Although we focused on the neurokinin-1 receptor, our findings are likely applicable to many G-protein coupled receptors because many of them show sustained signaling within cells, and therefore require drugs that can enter cells and block the receptors in endosomes,” said Bunnett.
Additional study authors include Alan Hegron, Chloe J. Peach, Raquel Tonello, Shavonne Teng, Rocco Latorre, Dane D. Jensen, Alex R. B. Thomsen, and Brian L. Schmidt of NYU College of Dentistry; Philipp Seemann, Harald Huebner, Dorothee Weikert, and Peter Gmeiner of Friedrich-Alexander Universität Erlangen-Nürnberg in Germany; and Jeanette Rientjes, Nicholas A. Veldhuis, Daniel P. Poole, and Wendy L. Imlach of Monash University in Australia.
Source:
Journal reference:
Hegron, A., et al. (2023) Therapeutic antagonism of the neurokinin 1 receptor in endosomes provides sustained pain relief. PNAS. doi.org/10.1073/pnas.2220979120.
