In a latest article revealed within the journal PLOS Medication, researchers carried out a potential, longitudinal research to estimate the proportion of outpatient consultations leading to inappropriate antibiotic prescriptions in younger kids in three low- and middle-income nations (LMICs), Madagascar, Senegal, and Cambodia.
Moreover, they robustly documented illness signs and diagnoses in these kids whereas evaluating antibiotic wants throughout every session.
 Research: Inappropriate antibiotic prescribing and its determinants amongst outpatient kids in 3 low- and middle-income nations: A multicentric community-based cohort research. Picture Credit score: okskaz / Shutterstock
Research: Inappropriate antibiotic prescribing and its determinants amongst outpatient kids in 3 low- and middle-income nations: A multicentric community-based cohort research. Picture Credit score: okskaz / Shutterstock
Background
The worldwide burden of bacterial illnesses is disproportionately massive in kids, particularly in rural settings of LMICs. Antibiotic overuse and inappropriate antibiotic prescribing drive antibiotic resistance, a worldwide public well being concern. Thus, characterizing inappropriate antibiotic prescribing amongst younger outpatient kids in LMICs is essential. At current, related information from LMICs, the place most inappropriate prescribing happens, on the neighborhood degree are scarce. Additionally, the seasonality of inappropriate antibiotic prescribing in LMICs is poorly documented.
In regards to the research
Within the current research, researchers recruited all kids from the BIRDY cohort who had at the least one outpatient session throughout their follow-up, starting from six to 24 months from baseline. They acquired systemic antibiotics administered through intramuscular, oral, or intravenous routes. BIRDY, a potential, long-term, community-based mother-and-child cohort research, happened in city and rural areas of Madagascar, Senegal, and Cambodia and estimated the incidence of antibiotic-resistant bacterial infections in kids beneath two years.
First, the researchers calculated the principle traits of the research inhabitants in every nation, together with the variety of consultations, diagnoses, antibiotic prescriptions, and inappropriate antibiotic prescriptions.
Subsequent, they categorized all diagnoses made by the doctor at every session utilizing a syndromic algorithm based mostly on Built-in Administration of Childhood Sickness (IMCI) tips of the World Well being Group (WHO) to find out all infectious diagnoses. Likewise, they used a two-step standardized classification algorithm to find out which well being occasions required antibiotics.
Throughout kids consultations, docs inappropriately prescribed antibiotics to many kids, even for well being occasions that didn’t require antibiotic remedy. Furthermore, some kids acquired a number of diagnosesmultiple antibiotic prescriptions throughout a session.
Thus, on this research, the researchers thought-about the variety of kids consultations not requiring antibiotics and the variety of antibiotics prescribed throughout consultations however not requiring antibiotics as distinct outcomes.
Additional, they used chi2 or actual Fisher assessments to check nations on qualitative and quantitative variables, with the importance threshold of all bilateral assessments set at 0.05.
Moreover, the researchers evaluated threat elements for inappropriate antibiotic prescribing, accounting for the historical past of the well being occasion, severity rating, season, and a toddler’s age.
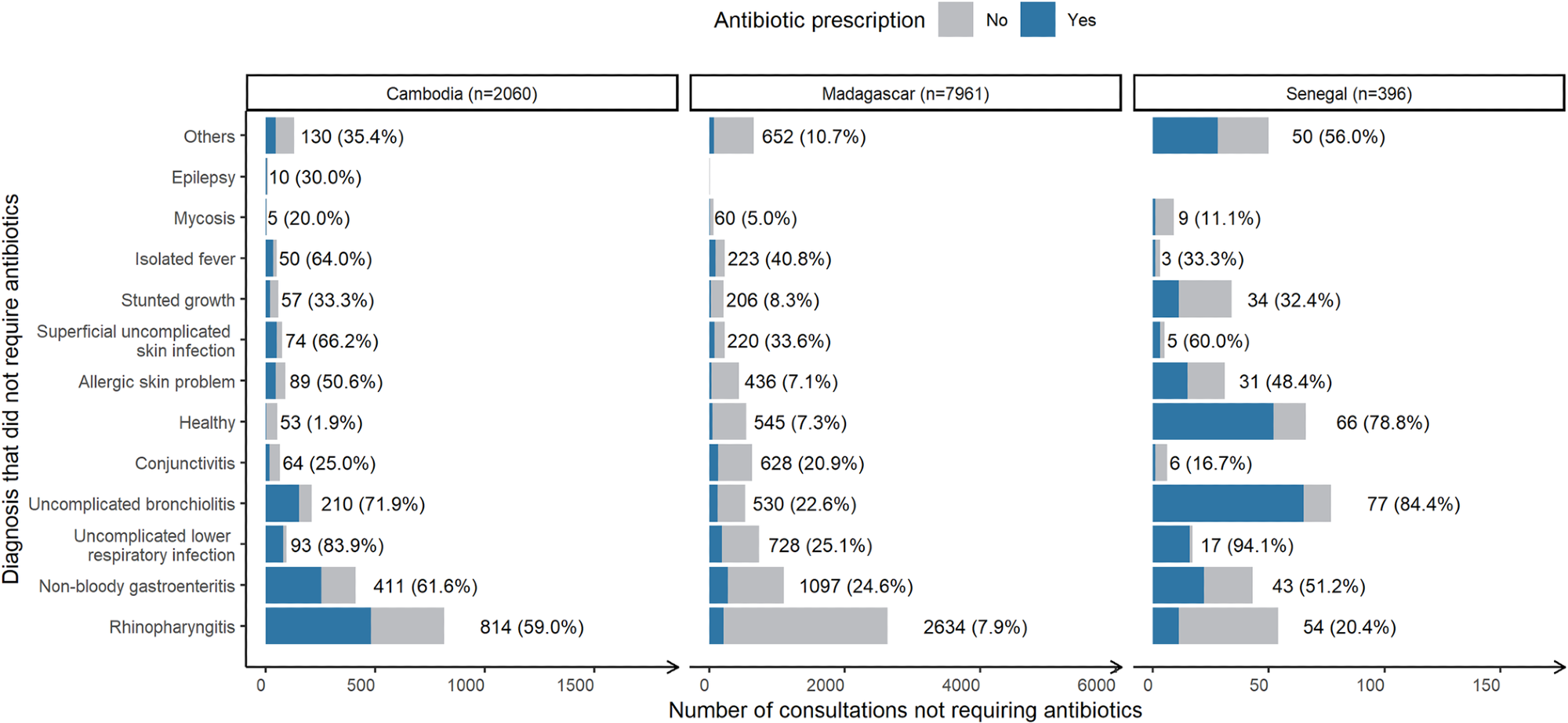 Variety of consultations “not requiring antibiotics” stratified by nation, related analysis and the share leading to antibiotic prescription (blue). Throughout all nations, N = 10,416. *Variety of consultations with this analysis (proportion leading to antibiotic prescription).
Variety of consultations “not requiring antibiotics” stratified by nation, related analysis and the share leading to antibiotic prescription (blue). Throughout all nations, N = 10,416. *Variety of consultations with this analysis (proportion leading to antibiotic prescription).
Outcomes
Almost 1 / 4 of outpatient consultations didn’t require antibiotic remedy; nonetheless, they resulted in an antibiotic prescription. Equally, three-quarters of all kids consultations ending up in antibiotic prescriptions had been inappropriate, and roughly two-thirds of these prescribed for younger kids had been pointless. Whereas these inappropriate antibiotic prescriptions offered little to no profit, they inadvertently harmed these younger kids by contributing to the emergence of antibiotic resistance.
Additional, the research outcomes advised that inappropriate antibiotic prescribing is frequent however extremely heterogeneous throughout nations. Accordingly, whereas solely 16% of consultations not requiring antibiotics resulted in antibiotic prescriptions in Senegal, the figures for Cambodia had been a lot greater, i.e., ~57%.
On this research, researchers documented all illness episodes microbiologically. They famous that 36% of kids acquired antibiotics even when their diagnostic assessments detected no pathogens within the stool. The truth is, docs prescribed antibiotics inappropriately for kids with gastroenteritis in 24.6%, 51.2%, and 61.6% of instances in Madagascar, Senegal, and Cambodia, respectively.
Likewise, the authors famous that almost one-fourth of all decrease respiratory tract an infection(s) consultations, primarily for bronchitis, ended up in inappropriate antibiotic prescriptions in Madagascar however >80% in Senegal and Cambodia. This quantity, nevertheless, remained beneath 60%, i.e., at 59% and 20.4% for rhinopharyngitis consultations in Cambodia and Senegal, respectively, and was barely at 7.9% for Madagascar.
The authors made one other placing statement in Senegal amongst kids consultations reported as wholesome but leading to antibiotic prescriptions. These diagnoses had been fairly widespread, happened on the supply of a new child, and 87% occurred in rural areas. This sample displays native session and prescribing conduct in Senegal, thus, requires cautious interpretation.
Essentially the most prescribed antibiotic to younger kids in Madagascar and Cambodia was amoxicillin, which docs prescribed in 24% and 35.7% of consultations, respectively, and cefixime in Senegal, prescribed in 34.4% of all kids consultations. The selection of antibiotics was comparable in Cambodia and Madagascar relative to Senegal.
All-cause antibiotic prescribing ranged between 20% and 60% for all three LMICs evaluated on this research. Neither various research designs and protocols nor variations in infectious illness burden clarify these noticeable intercountry variations in kids consultations.
The authors additionally recognized some key determinants and patterns of inappropriate antibiotic prescribing throughout all three LMICs.
First, they famous that kids older than three months than youthful infants had been at a better threat of receiving an inappropriate prescription, doubtless as a result of they’re extra susceptible to contracting extreme bacterial infections. Second, they famous that medical severity scores elevated the danger of inappropriate antibiotic prescription. In some instances, physicians prescribe inappropriate antibiotics as a result of dad and mom appear overly involved and categorical extra frequent or extreme illness signs.
Third, the authors famous that kids’s consultations within the wet vs. dry season extra doubtless resulted in inappropriate antibiotic prescriptions. Fourth, they discovered that kids inhabiting rural areas had been at a better threat of getting inappropriate antibiotic prescriptions, doubtless as a result of practitioners working in rural settings are normally much less certified. Word that tradition, socioeconomic situations, and healthcare practices (not simply the illness burden) largely decide intercountry variations within the amount and lessons of antibiotics bought. Nevertheless, because the researchers analyzed drug gross sales information on this research, it offered restricted data on this context.
Conclusions
The present research offered a extra detailed and correct image of inappropriate antibiotic prescribing to kids throughout all three LMICs. Thus, this research highlighted the necessity for focused interventions to stop these practices, reminiscent of coaching prescribing clinicians about legitimate pediatric medical administration tips, e.g., IMCI tips, an intervention that dramatically lowered inappropriate antibiotic prescribing in some African nations, e.g., Uganda. Equally, speedy diagnostic testing may assist physicians, particularly these working towards in distant areas, perceive whether or not a illness has viral or bacterial etiology and prescribe antibiotics appropriately.
In conclusion, the research outcomes remarkably confirmed that the decision-making course of governing antibiotic prescription is complicated; thus, physicians ought to search microbiological data and never deviate from established tips earlier than prescribing antibiotics to kids. Future sociological and qualitative research may facilitate a greater understanding of the perceived necessity of antibiotic prescribing in high-risk populations of LMICs.
Journal reference:
- Inappropriate antibiotic prescribing and its determinants amongst outpatient kids in 3 low- and middle-income nations: A multicentric community-based cohort research, Antoine Ardillon, Lison Ramblière, Elsa Kermorvant-Duchemin, Contact Sok, Andrianirina Zafitsara Zo, Jean-Baptiste Diouf, Pring Lengthy, Siyin Lach, Fatoumata Diene Sarr, Laurence Borand, Felix Cheysson, Jean-Marc Collard, Perlinot Herindrainy, Agathe de Lauzanne, Muriel Vray, Elisabeth Delarocque-Astagneau, Didier Guillemot, Bich-Tram Huynh, On behalf of the BIRDY research group, Plod Medication 2023, Printed: June 6, 2023 DOI: https://doi.org/10.1371/journal.pmed.1004211, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1004211
